Corneal Transplant
The cornea is the transparent front part of the eye that allows light to enter the eyes. It covers the iris, pupil, and anterior chamber. Along with the lens, it refracts light rays to bring them to focus onto the retina and accounts for approximately two-thirds of the total optical power of the eye. When it loses its transparency it affects the vision of the eye.
Corneal transplantation, also known as corneal grafting, is a surgical procedure wherein a damaged or diseased cornea is replaced by donated corneal tissue (the graft). When the full thickness of cornea is replaced it is known as penetrating keratoplasty and when partial thickness of the cornea is replaced it is known as lamellar keratoplasty. The graft is harvested from a recently dead individual with no known diseases or other factors that may affect the survival of the donated cornea or the health of the recipient.
Indications for Corneal Graft
- Optical: Graft may be required to improve visual acuity by replacing the opaque or distorted host cornea by a clear healthy donor tissue. The most common indication in this category is pseudophakic bullous keratopathy, followed by keratoconus, corneal degeneration and dystrophies, as well as scarring due to keratitis and trauma.
- Tectonic/reconstructive: To preserve the anatomy and integrity of the cornea in patients with stromal thinning and descemetoceles, or to reconstruct the anatomy of the eyeball, e.g. after corneal perforation.
- Therapeutic: To remove inflamed and infected corneal tissue that is unresponsive to treatment by antibiotics or anti-virals.
- Cosmetic: To improve the appearance of patients with scarred white corneas.
Procedure
A thorough history taking and eye examination is done much before the actual surgery, including an ophthalmic ultrasound to assess the posterior segment, where it is not visible. This helps the ophthalmologist form a diagnosis and also assess the prognosis for visual recovery. Sometimes a grafting surgery may be combined with a cataract surgery and/or other procedures depending upon the findings of the pre-operative examination.
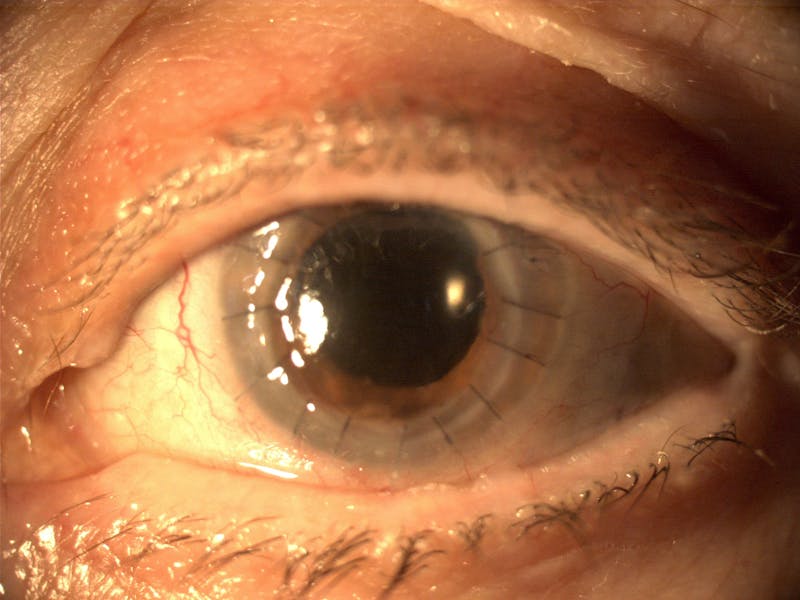
Penetrating keratoplasty
A trephine (a circular cutting device) is used to remove a circular disc of cornea, from the donor cornea. Then a second trephine is used to remove a similar-sized portion of the patient’s cornea. The donor corneal tissue is then sewn in place with sutures.
After instilling antibiotic eye drops, the eye is patched and the patient is taken to a recovery area. The patient typically goes home after a while and has a follow up visit on the following day for the first postoperative appointment.
Lamellar keratoplasty
Lamellar keratoplasty involves selectively replacing the diseased layers of the cornea while leaving the healthy layers in place. The chief advantage is this procedure is the improved tectonic integrity of the eye. The main disadvantage is the technically challenging nature of these procedures, which involve replacing portions of a structure that is only 500 μm thick, and compromised optical performance of the donor/recipient interface compared to full-thickness keratoplasty. There are several techniques of lamellar keratoplasty:
Deep anterior lamellar keratoplasty
In this procedure, the anterior layers of the central cornea are removed, leaving the endothelial cells and Descemet’s membrane in place. Donor tissue replaces the removed anterior layers of the cornea. This technique is used in cases of anterior corneal opacifications, scars, and ectatic diseases such as keratoconus.
Endothelial keratoplasty
This involves replacing the patient’s endothelium with a transplanted disc of posterior stroma/Descemet/endothelium (DSEK) or Descemet’s/endothelium (DMEK).
It is a relatively new procedure and has revolutionized treatment of disorders of the innermost layer of the cornea (endothelium). The surgery can be performed with one or no sutures, unlike a full-thickness corneal transplant, that requires multiple sutures. There is earlier recovery of functional vision (days to weeks), as opposed to up to a year with full thickness transplants.
Risks of Corneal Grafting
There is a risk of corneal rejection and primary graft failure. Corneal graft rejection occurs in about 10% of cases. Graft failure can occur at any time after the cornea has been transplanted, even years or decades later. The causes can vary, though it is usually due to new injury or illness. Use of immunosuppressants, including cyclosporine A and tacrolimus, helps prevent graft rejection.
Certain risks are peculiar to lamellar keratoplasties, like detachment or displacement of lamellar transplants.
There is also a risk of infection, since the cornea has no blood vessels. Therefore it heals much more slowly than a cut on the skin. The slow healing makes it prone to infection by various microorganisms. This risk is minimized by antibiotic prophylaxis. The infection could also be of the interior of the eye.
Minor complications can occur but do not usually affect the result. These include raised pressure in the eye or a leak of fluid between the stitches. Occasionally, if the leak does not seal on its own, an extra stitch or replacement stitch is required.
Other risks and complications include, but are not limited to:
- Bleeding
- Glaucoma (increased pressure inside the eye)
- Cataract formation
- Detached retina (tissue lining the back of the eye pulls away from the eye)
- Visual acuity problems (sharpness of the vision) caused by an irregular curve in the shape of the cornea
DISCLAIMER
This web page provides general information and discussions about health, medicine and related subjects. The information and other content provided on this website, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment.
The content is for information purpose only and is not a medical advice. Qualified doctors have gathered information from reputable sources; however Credence Medicure Corporation is not responsible for errors or omissions in reporting or explanations. No individual should use the information, resources and tools contained herein to self diagnose or self treat any medical condition.
If you or any other person has a medical concern, you should consult with your health care provider or seek other professional medical treatment. Never disregard professional medical advice or delay in seeking it because of something that have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or emergency services immediately.
The opinions and views expressed on this blog and website have no relation to those of any academic, hospital, health practice or other institution. Credence Medicure Corporation gives no assurance or warranty regarding the accuracy, timeliness or applicability of the content.
